Cochlear implants in children
Authors: David Horn, Hitomi Sakano
Contributors: Diane Lazard, Rémy Pujol
Cochlear implantation (CI) in deaf children involves unique challenges compared to post-lingual adults. In adults whose brains have been shaped by acoustic sound perception, the success of the CI may primarily depend on how well the implant provides pre-deafness auditory resolution, and how the brain compare the new signal with what has been previously heard. In children, however, the auditory system is immature at the time of deafness and restoration of hearing with a CI. Development of the auditory system then proceeds in the presence of an atypical signal that is significantly different relative to the normal signal. Consequently, CI success depends on the time of implantation.
History/Critical Period
For a general history of the development of cochlear implant technology, refer to the previous page ‘ Cochlear implants: overview‘.
It is known that in animals, there is a “critical period” (also called “sensitive period”) during which sensory input is necessary for the proper formation of the visual and auditory cortex. After this period, restoration of sensory input in deprived animals does not result in proper sensory perception. In humans, there is substantial data from children who have received a CI at various ages suggesting that earlier implantation results in better outcomes in speech perception and language tasks. On average, children implanted later than 2 years of age show poorer outcomes than children implanted earlier than age 2.
Considerations for CI in children: assessing candidacy
Before consideration of CI, thepatient meets with a team of experts including the surgeon, audiologist, speech therapist, and genetic counselors. Throughout the process, there should be involvement of their parents, pediatrician and teachers.
Cadidacy considerations, in the USA, include the following: age 12mo-17yrs, profound SNHL, minimal benefit with hearing aids, not meeting auditory milestones, no evidence of central auditory lesions. As with any surgery, the patient/family should desire to undergo surgery and have a realistic expectation of outcome. In the USA, CI is currently FDA approved at age 12mo for profound and 18mo for severe SNHL, however the candidacy criteria is continually changing with the improvement in CI technology and with increasing data supporting the benefit of early implantation.
All pediatric CI candidates require some imaging of the temporal bone to assess surgical anatomy, particularly patency of the scala tympani.
Cochlear Implant Surgery
Device components and implantation
As for the adults, the CI device consists of two parts:
an internal part (electrode and magnet)
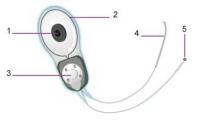
an external part (receiver)

Legend: 1) magnet, 2) antenna, 3) stimulator, 4) multi-electrode array, 5) ball electrode, 6) microphone, 7) speech processor, 8) magnet, 9) transmitting coil
How the device works ?
S. Blatrix
Surgical consideration
As with any surgery there are potential complications, and those associated with this particular procedure include hematoma, local infection, dizziness, and tinnitus. Children with CI may have a higher risk of developing otogenic meningitis, particularly streptococcal meningitis. CI candidates with atypical temporal bone anatomy, previous history of meningitis, CSF leak at time of surgery, or those with certain types of surgical positioners may be a particularly high risk. Thus, pneumococcal vaccination is recommended in all pediatric CI recipients (link to CDC vaccination recs for CI recipients: http://www.cdc.gov/vaccines/vpd-vac/mening/cochlear/dis-cochlear-faq-hcp.htm). Less common complications include CSF leak, facial nerve injury, and extrusion of hardware. To minimize risks, surgery is deferred in the setting of an active infection, i.e. OM. In children with chronic otitis, typically ventilation tubes are placed and then surgery is performed when the middle ear is dry.
Revision Surgery
Revision surgery rates vary between 5 and 12%, and are most commonly attributed to device failure. Other reasons may include poor wound healing and device extrusion. With any replacement of implant, one should consider the potential for further hearing loss due to repeat cochlear trauma.
Rehabilitation (see also specific page)
After the immediate recovery from CI, patients will meet with audiologists for programming of their implant. They will also require ongoing rehabilitation with speech therapists and close involvement with their teachers.
Future of Cochlear Implantation in Children
Simultaneous versus Sequential Bilateral Cochlear Implantation
Studies suggest that speech perception is improved after the second CI compared to single implantation alone. Improved localization and speech understanding in noisy background has been demonstrated in adults and there is emerging evidence for similar benefits in children. Furthermore, sequential implantations at earlier ages (<5) and at shorter intervals are suggested to have better outcome. Although sequential implantation at longer intervals (several years) still improves speech perception and learning, the outcomes decline with increasing age at second implantation. Given these results, more infants are now being implanted sequentially at shorter intervals (<12months) or even simultaneously. There is however strong evidence for single CI coupled with hearing amplification on the contralateral side to achieve bilateral input.
Relaxation of Candidacy Criteria
Although CI is a treatment for severe to profound SNHL, hearing loss is often associated with anatomical malformations that have formerly been contraindications for CI due to the inconsistent benefit of CI on speech perception in these patients. However, the criteria for CI candidacy are slowly being expanded to include abnormalities such as cochleovestibular anomalies and cochlear nerve deficiency, as well as auditory dyssynchrony/neuropathy where neural signals from intact cochlea are not properly conveyed to the brain. Although outcomes of CI in these children vary widely, the hope is that these patients will at least benefit from auditory awareness even if they do not achieve speech perception.